Introduction
Health organizations are under pressure to use the best electronic applications for their healthcare data, but as technology rapidly changes, many are left with the issue of what to do with legacy data. How do you archive the data in a way that keeps your organization compliant, protected from security risks, and easily accessible for patients? Our guide on legacy data management in healthcare aims to answer those questions.
Health data is tripling every three years, leaving health organizations grappling with the challenge of managing an exorbitant amount of new data while at the same time maintaining multiple legacy data systems. This is not a new issue in the health industry, but with the rise of cyberattacks and new health data laws, not to mention mergers and acquisitions growing data within organizations and adding to a portfolio of applications, this is becoming an increasing priority for health organizations.
As an expert in health data management, we’ve designed an in-depth guide going over the basics of legacy health data management, breaking down the challenges and benefits to this process. We’ve also put together a free downloadable checklist complete with the steps you can follow to come up with an actionable plan to protect your data well into the future.
What is Legacy Health Data Management?
Legacy data is defined as older information that is necessary to an organization, but is housed within an inaccessible or outdated system, format, or technology source. So, what is legacy health data management? Legacy health data management is the manner of capturing, organizing, analyzing, and storing historical electronic health records (EHRs) and other data in healthcare organizations to support data-driven decision-making processes.
In our survey of Chief Information Officers (CIOs) at healthcare provider organizations, 94% shared they are still operating on legacy applications. These legacy systems can be filled with decades of data. The first EHRs were introduced and implemented in the medical field in the 1960s although they didn’t become more widely accessible until decades after that.
Currently, health organizations are facing increasing pressure to end their reliance on these outdated legacy systems to protect, retain, and improve the accessibility of data. However, it needs to be done in a way that keeps up with rapidly changing technological advances, provides interoperability, as well as addresses the costs to get this work completed as smoothly as possible. This guide to legacy health data management is important now more than ever as healthcare organizations navigate the ever-changing digital health landscape.
“Healthcare delivery organizations of every shape and size must have a lifecycle data management strategy,” explains Harmony Healthcare IT CEO, Tom Liddell. “The plan should address risk mitigation, compliance requirements and support record sharing accessibility of the comprehensive medical record for years to come.”
Properly managing health legacy data leads to numerous positive changes within a healthcare organization including:
- Accessibility
- Compliance
- Interoperability & Integration
- Patient safety
- Data protection

“In our world, it’s a cost containment play,” explains Harmony Healthcare IT CEO Tom Liddell. “In that preservation of data, we’re helping people with migration. We call it archival. It’s really a transformative process that does that, ultimately reducing that cost and preserving that data.”
4 Challenges with Legacy Health Data Management
Properly managing health legacy data is not an easy undertaking. The average hospital uses 10 EHRs, and health systems use as many as 18 different EHRs. There are several reasons for adding new electronic health record systems despite already having one in operation. It could be because a newer EHR is offering better technology, or, in the case of a merger or acquisition, because the other organization uses a different one.
As health organizations strive to stay at the forefront of technology, legacy data management is key to providing medical professionals with what they need to do their jobs while also giving patients proper access to their health information. However, this comes with a host of challenges. Below are four common challenges we see when it comes to legacy data management in healthcare.
1. Security
One of the most common challenges with legacy data management is security. Over 4 in 5 (81%) CIOs say security is the top concern when using legacy applications, which is no surprise with cyberattacks becoming increasingly common, especially in the healthcare industry.
According to the 2022 FBI Cyber Crime Report, ransomware attacks in the healthcare and public health sectors saw a 42% increase from the year prior. Many legacy health data management systems have outdated security protocols, often lacking modern cybersecurity features necessary to keep sensitive patient information safe such as encryption and access controls. The data can also be stored in out-of-date servers vulnerable to attack.
2. Accessibility
Accessibility is a common issue for these older healthcare systems and interfaces because they may be operating with software that isn’t widely used or updated and lacks user-friendliness. Inaccessible data not only negatively impacts patients’ access to their medical records but the lack of easy clinical access to historical information can make it harder for providers to make informed, data-backed decisions for their patients. This can impact release of information (ROI), as well as compliance. If accessibility becomes too difficult, health organizations may be forced to retire an application.
3. Compliance
Legacy data often needs to be kept for compliance, however, older applications can run the risk of not meeting requirements because many are often outdated and have limited interoperability. On top of needing to meet each health organization’s internal policies, legacy data applications also need to meet all health laws such as federal and state record retention laws, HIPAA rules, and the 21st Century Cures Act which requires patients have more instant electronic access to their health data. This can be hard to provide if the application is technologically obsolete and not receiving the proper updates or security measures necessary for data protection.
4. Cost
Continuing to keep health legacy data applications up and running means footing the bill for regular software and hardware maintenance to make sure that your legacy system stays in compliance. Over half (55%) of CIOs who use legacy applications cited IT labor burdens as a frustration when dealing with these applications. Maintenance for these legacy applications can lead to a 15% annual budget increase. Legacy systems also cost time and money in training, so workers can retain access and know how to use the system. And while data archiving may have a cost, it usually pays itself off quickly when you consider all of these added costs.
The growing volume of health data means there needs to be increased data agility and plans in place for legacy data management before a company finds itself struggling with major security risks, compliance, or costs. Addressing data shortfalls and solidifying plans to face these challenges early can help avoid future stressful situations.
In one instance, a healthcare provider in California found itself in a bind while trying to archive 27 terabytes of dental records to save costs and improve accessibility. The project was at a standstill and at risk of falling out of compliance when our team stepped in to help fix the problem. Here is where an active archive for legacy records can provide a big benefit.
Benefits of Legacy Health Data Management
Why should a healthcare provider organization implement a robust legacy health data management strategy? In short, effectively managing legacy applications will lessen the burden for application users, the greater health organization, and of course, patients. If done right, a well-operated legacy data management plan makes everyone’s jobs easier. Below are some of the specific ways it helps people working in different roles in the healthcare system.
Legacy health data management benefits for users
- Enhanced efficiency
- Reduced burden for clinicians
- Improved release of information workflows
- Simplified reporting
For users, specifically clinicians, a well-implemented health legacy data plan that includes a consolidated active archive for historical records is key to improving day-to-day operations because it improves their daily processes and workflow. Users can find records faster when working on a system with an inherently easy user interface which in turn helps with the retrieval of patient medical records. For example, when helping with data consolidation for the Torrence Health Association in California, our archival work helped move six legacy systems into one single archive. This made it easier for users to access historical records.
Successful legacy health data management can also automate repetitive administrative tasks and customize legacy systems, giving users more time to spend on patient care. Ultimately, these measures to improve pain points help to simplify users’ workflows.
Legacy health data management benefits for health organizations
- Consolidated data
- Enhanced efficiency
- Reduced cost
- Compliance with regulations
- Increased security
- Improved interoperability
The benefits of legacy health data management are unmatched for a wider health organization. While completing data consolidation for a major merger and acquisition for a Northeast integrated healthcare system, our legacy data management work helped save more than two million dollars by reducing costs from vendors to IT and others.
When correctly done, this can and will impact workers in roles spanning from finance to human resources to IT and accounts receivable. Proper legacy health data management consolidates data, supports compliance with regulations, cuts down on cost and risks to the organization, and improves interoperability. At a granular level, there are even more benefits of a streamlined application portfolio that leverages an active archive.
Accounts Receivable
- Allows for A/R wind down
- Reduces software application costs
- Supports record retention and compliance
Compliance & Legal
- Data consolidation makes it easier to ensure compliance
- Cuts down on legal risks and liabilities
- Improves security, protecting sensitive health data
Finance
- Decreases annual application and hardware maintenance costs
- Reduces training costs for staff
- Improves overall ROI
Health Information Management (HIM)
- Simplifies Release of Information workflows of historical records
- Interoperability helps with data exchange
- Assists in compliance
Human Resources
- Helps maintain and track employee data
- Ensures HR data meets federal & state requirements
- Streamlines insurance and worker compensation claims
Information Technology (IT)
- Alleviates burden of maintaining old, outdated systems
- Decreases cybersecurity risk
- Supports data integration due to improved interoperability
Mergers and Acquisitions (M&A)
- Helps achieve a faster return on investment (ROI)
- Supports data compliance and reduces legal risk
- Improves interoperability to help with data sharing and accessibility
Research
- Consolidates historical patient data to one location
- Simplifies process of accessing legacy health data
- Data standardization helps improve analyses
Legacy health data management benefits for patients
- Supports continuity of care and diagnostic accuracy
- Empowers patients
- Improves access to comprehensive health history
Legacy data management in healthcare is key to ensuring patients receive the best treatment possible when it comes to their health. In fact, not only is this something patients should have, but it’s something they demand. Having easy access to their comprehensive health history empowers patients to take ownership of their health without having to rely on others.
The 21st Century Cures Act further empowers patients through its three main tenants: Patient Access, Protection and Choice. This means patients have the right to control their own health care and can access their medical records through smartphones and modern software apps. It also protects their privacy with secure protocols like those used in banking and travel apps. Plus, it expands patient and payer choice by insisting on increased transparency for costs. Most Americans want their data to be more accessible and better protected, according to a national survey for The Pew Charitable Trust.
When clinicians and medical professionals can easily see their patient’s holistic healthcare history it improves the continuity of care leading to a better patient experience. This in-depth data will ensure the patient doesn’t undergo redundant or unnecessary test procedures. It also helps improve the medical diagnosis process and helps doctors determine ideal medication plans based on what has worked best in the past.
An archive benefits clinicians and patients. A consolidated archive supports more informed patient care, improved outcomes and data interoperability – getting health data to all the places it is needed. This includes better release of information and access to historical records. When a healthcare provider has an archiving strategy in place, Secure Record Delivery from an archive integrator platform can support the inclusion of a defined HIPAA designated record set, including data from the archive to an endpoint that provides patients with a copy of their full clinical narrative.
3 Foundational Steps to Developing a Legacy Data Management Strategy in Healthcare
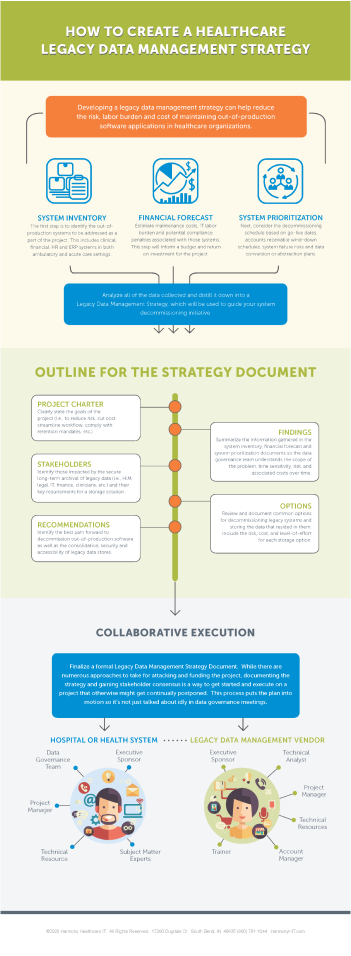
Before moving forward with a legacy data management plan, health organizations need to solidify their strategy with these three foundational steps. These are crucial to creating an indispensable legacy data management plan.
Step #1 – Establish a Data Governance Team
The first step to develop a legacy data management strategy in healthcare should be to establish a data governance team. A data governance team is a group of employees across departments within the organization whose goal is to create company-wide policies and processes about data. This includes decisions on data accuracy, security, and interoperability. There are seven key steps this team should follow when it comes to implementing strong data governance for legacy data:
- Foster cultural acceptance
- Choose sponsors for legacy applications
- Identify project manager
- Distinguish data lifecycle pathways
- Track progress
- Solidify data strategies and policies in playbook
- Promote communication
You can learn more about these steps and how data governance teams help provide support and assistance when it comes to healthcare data management in our data governance guide.
Step #2 – Create a System Inventory
Next will be to create a system inventory to determine which legacy applications are useful. This inventory will help organize and determine every system the health organization has under its management. This is a crucial step because health systems, especially larger ones, could have hundreds of systems to keep track of everything from clinical, inpatient, and outpatient work to ancillary, financial, and administrative documentation.
After organizing the number of legacy systems in existence, the team will need to go deeper and gather the details of each system and its data. It is important to know how information is stored, where the data is located, and how long it must be retained. During this part of the process, subject matter experts (SMEs) should be looped in to ensure system processes are accurately understood. They will also be key individuals to work with when changes are made to legacy systems because they’ll be able to verify all data is correctly managed during an archival process.
Step #3 – Acknowledge Problem
After examining the organization’s collection of applications and understanding the associated challenges and risks, the next step is acknowledging that there is a problem that needs to addressed. Socializing this internally with key decision makers and influencers is key to getting the support needed to create and implement a plan to address the problem. As you get deeper in your strategy development, you’ll be provide more supporting details and benefits, but it is ideal to start gaining support early in the process, and ideally an Project Sponsor that will be a champion for the initiative.
Legacy Health Data Management Options
After taking the foundational steps to fully understand the data landscape, it’s up to the health organization to choose how to go forward when it comes to addressing its legacy data. There are four main paths companies can choose to take: maintaining legacy systems, converting legacy data to an EHR, archiving legacy data to a PDF, or archiving legacy data discretely.
We’re providing pros and cons below for each option, however, based on our experience, we strongly recommend archiving legacy data discretely as a best practice when decommissioning a system with historical data.
Maintain Legacy Systems
Pro: If the decision is made to maintain legacy systems you will not have to overhaul the current system, and all employees will not have to be retrained on a new system.
Con: Maintaining legacy systems leaves your organization open to security vulnerabilities. On top of legacy vendor costs and the budget needed for continued maintenance, this system may also not be able to meet necessary security efficiency requirements putting you at risk for non-compliance. Another pain point is that employees will need to manage multiple system logins and will need continued training on the outdated system to ensure no accessibility is lost.
Convert Legacy Data to EHR
Pro: Data will be operating on the go-forward EHR platform for easy access and better functionality.
Con: While this may seem like a good option, the process of converting data to an EHR is complex and costly. It requires in-depth data mapping and takes time. Therefore, all the data may not be accessible when the new EHR goes live, running the risk of not meeting compliance or efficiency requirements.
Archive Legacy Data to PDF
Pro: By archiving legacy data into PDFs, it will be available in a format that is widely accessible to all.
Con: Moving legacy data into PDFs buries data into pages and removes structured data. That can make it less searchable and, therefore, more difficult for users to access and review. On top of that, it can lead to interoperability issues and make it so the data does not meet accessibility or privacy requirements.
Archive Legacy Data Discretely
Pro: Archiving records discretely in an active archive enables data sharing, making it easy to access the data, sort/filter it, release it, and look through the analytics. The process also meets all security and privacy requirements along with compliance, accessibility, and efficiency requirements.
Con: This process will incur costs for health organizations, but it can quickly pay itself back in both hard and soft cost savings.
Archiving legacy data discretely is often the best choice for organizations as it provides the best value with its ability to save costs and serve the needs of the involved departments.
Legacy Health Data Management Checklist: Archiving
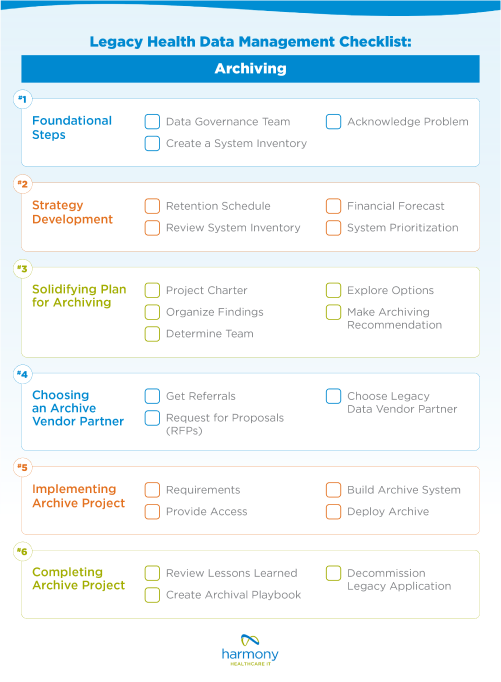
So, what are the necessary steps to solidify your legacy health data management plan? We put together a checklist to help you stay organized, making it easy to ensure nothing is forgotten about during this process. While it may not seem like your legacy data needs to be managed or adjusted right this moment, it’s important to keep in mind there are multiple reasons records can and will be needed in the future. This checklist will ensure you are prepared when that time comes.
Strategy Development
Once you’ve decided that archiving is the right solution for your organization, there are some steps to take before delving straightaway into the archiving process. You need to strategize and create an in-depth plan. While this part of the process takes time at the forefront, it will ensure you avoid roadblocks during the archival process in the future.
Retention schedule
Make sure that you have an in-depth retention schedule. This documented plan should include how long you’re keeping health data records before securely disposing them or archiving them. It should also include the processes for managing and storing this data including whose job it is to regularly monitor and implement these changes.
Review system inventory
In the foundational steps of legacy data management, we talked about the need to put together a system inventory. Before making any major changes to your legacy data you’ll need to review your system inventory again. Triple check that all of your organization’s current systems are listed and review the concerns associated with any applications. This will assist your team when making your application rationalizations.
Financial forecast
Before moving forward with decommissioning or changing any legacy health systems, you also need to know that you have the funds to do so which is where a financial forecast comes in. A financial forecast should be done to estimate the overall cost to changes with any legacy systems, allocations needed to get the job done, and an expected ROI. This will also help communicate to any stakeholders the overall budget and the most important initiatives if all funding is not available at once.
System Prioritization
With numerous legacy systems in place, you’ll need to go through and prioritize your systems. Organize the legacy systems based on categories such as cost, contract renewal dates, retention mandates, and risk such as security concerns. This will help give you a better idea as to which systems you should prioritize making changes to and which ones will be best to leave be for the time being.
Solidify Plan for Archiving
There are five steps to focus on while drafting your legacy data management strategy that includes archiving. These will help you organize your plan, including the reasons why changes need to be made to your legacy data now.
Project Charter
The project charter is similar to creating a thesis before writing a paper. This should include your overarching goals, reasons for the project, and expected benefits all in one place.
Organize Findings
The findings should be a more in-depth part of your strategy, describing how long you expect the implementation/changes to take, along with the anticipated budget and scope.
Determine Team
You’ll need to determine the team needed to execute the legacy data management strategy. This includes a dedicated program manager as well as an executive-level champion, which is the person who will advocate and support the project. Alongside those positions, you’ll also need to determine key people from different departments such as IT, HIM, compliance, legal, and others needed to support the project.
Explore Options
This strategy needs to include all options for archiving your legacy data. You should consider hosting options and pricing model needs.
Make Archiving Recommendations
Finally, you’ll need to come up with your main recommendations for your legacy data management plan. These recommendations should include the preferred hosting solution, a timeline for implementation, the anticipated costs, along with any potential risks that could come up on the way.
Choosing an archive vendor partner
From here, you’ll need to choose a legacy data vendor to partner with to make these changes. Ideally, you want a vendor with the products along with the skills and experience to complete your project within budget and with a proven record of ROI. The legacy data vendor should have a clear method of implementation, should be able to provide customization to fit your needs, and have the expertise to guide you and your health organization. Other aspects to keep in mind when choosing the right legacy data vendor partner are:
- Referrals from other healthcare colleagues
- Industry Rankings such Gartner and the KLAS Software and Services Report
- HITRUST certification to ensure they prioritize cybersecurity
- Request for Proposal (RFP) to compare vendors
Implementing archive project
Once you’ve settled on a health data vendor your archive project can officially start with four final steps below. The best part about this process is now that the pre-work has been completed, you should be able to repeat the steps below for future archiving projects.
1. Requirements
Now that you have a data vendor selected, you’ll need to work with your partner to determine full requirements in order to solidify the scope and plan to address the legacy data.
2. Access
From there, access to the legacy data will need to be given to your vendor. This will give them the ability to begin archiving your legacy systems properly.
3. Build
Now the work truly begins. The next steps will be to begin developing an archive infrastructure and user interface. This part of the archiving process requires of validation to ensure data is being archived correctly and compliantly.
4. Deploy
Finally, the deployment is what happens when the archived legacy systems are rolled out. Employees will need to be trained to learn how to access the legacy data.
Other Services to Consider for Legacy Data Management in Healthcare
We’ve become experts in the unique barriers health organizations can face while archiving data and worked hard to come up with solutions and services to make the archiving process as seamless as possible. Here are some special considerations to keep in mind for legacy data management.
Records Release Service
A records release service streamlines any requests for medical or business records for patients, lawyers and others who have a legal right to these records. The service is especially useful if a health organization is facing closure or in the process of an M&A. Using a records release service ensures compliance with all healthcare regulations and provides a simple, streamlined solution for those in need of their records.
Secure Record Delivery

When patients request their medical records, they have a right to get access to all of their electronic health information within a reasonable time period. Manually retrieving legacy data can lead to mistakes as well as delays. So, through HealthData Archiver®® we’ve created a Secure Record Delivery solution to circumvent these issues, improving interoperability. This system standardizes data from legacy systems and transmits historical charts straight to your patient portal or other EHR endpoint.
Patient Identity Management
A major issue in healthcare is making sure medical records match the correct patient. When consolidating legacy data into a central archive, patient identity management is vital to ensure medical records are linked to the right person. There are a few different ways to do this, from Single Sign-On to linking historical patient records to an MPI (master patient index).
Ongoing Archiving Process and Approach
Once you finish archiving health data, the work does not end there. As you know, there are numerous legacy systems in need of management and attention. After completing your first archive project from start to finish, the process can easily begin all over again with a new system. However, now that you’ve set the groundwork, you do not have to start from scratch.
As you prepare for future projects, discuss your lessons learned. Review what worked and what didn’t. Are there things you can change for the future? Or were these issues things that are out of your control? From here, you can create an archival playbook. Outline what systematic approaches work best for your health organization. Create your own guide to legacy data management to highlight the methods and strategies that work best when it comes to archiving legacy data in your organization.
Finally, go forward with decommissioning your legacy application. When you decommission your legacy system, everything should be complete with no loose ends. From there, the process can begin again, and this time with your additional experience and education the process will only get smoother.
Do you have legacy data to manage?
Let’s connect. We can walk through your unique needs and ensure you are set for the future.






