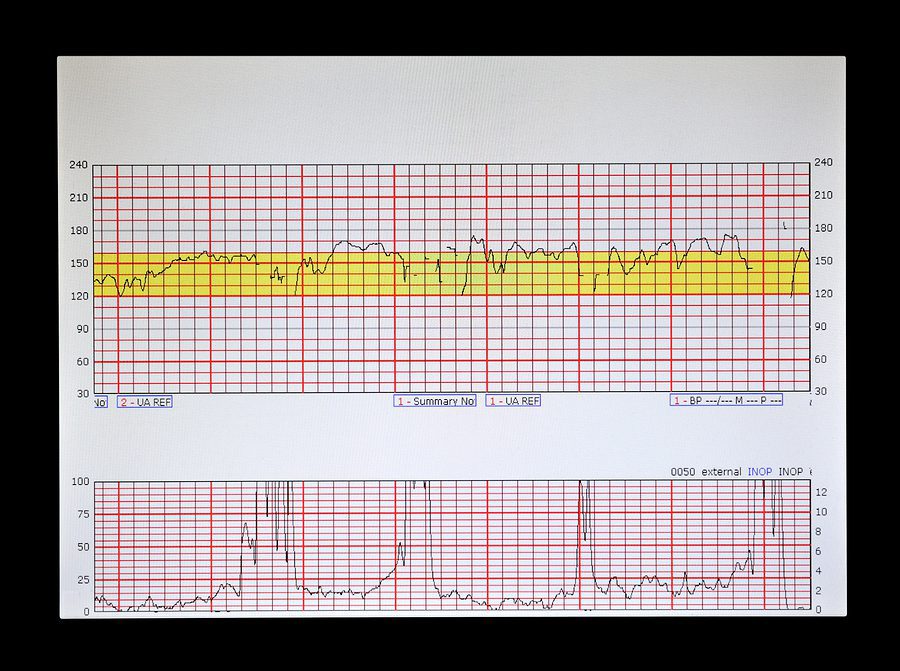
For over 50 years, electronic fetal monitoring (EFM) has played a critical role in assisting labor and delivery teams. In the early days, fetal monitoring strips – which indicate if, when and how long a fetus is in distress – were output to paper. But, with the emergence of perinatal data management systems years later (i.e., Phillips OB TraceVue, GE Centricity™ Perinatal system and PeriGen Watchchild®), the ability for hospital caregivers to see and store perinatal information in context with fetal monitoring strips in a digital format was born.
So, gone are the days of racking boxes of paper strips to meet medical record retention requirements. However, a best practice is now required for archiving digital fetal monitoring strips when an electronic perinatal system gets replaced, retired, or decommissioned. Because, if the data isn’t accessible when a legal release of information is requested, the penalties could be extensive.
Storing Fetal Monitoring Strips for Cases of Litigation
In cases of litigation surrounding traumatic delivery, fetal monitoring strips may be sought as evidence long after the initial date of birth. While retention requirements vary by state, fetal monitoring strips are often retained 10 years past the age of majority. 28 years is a long time, and the law leaves little leeway if fetal monitoring strips are not produced upon request.
As long as the plaintiff is able to show that relevant fetal monitoring strips existed, the hospital had control over them, and that the law was violated when the hospital failed to keep the strips, the court may either render a missing document charge or strike the defending hospital’s answer for spoliation of the evidence.
A missing document charge is most common of the two options and directs the jury to draw the strongest adverse conclusion from the missing strips when considering evidence against the defending hospital. The more severe consequence is if the court finds a spoliation of evidence, a default judgment is handed down against the hospital or provider. This determination is only available in limited circumstances and the plaintiff must prove that the loss of the EFM strips deprives him/her the ability to prove if the birth injury is the result of malpractice.
To avoid scrambling for data during litigation or for any request, it’s imperative for hospitals to put a strategy in place for fetal monitoring strip retention, storage, and accessibility, especially when there’s upcoming intent to replace a legacy system with a new EHR.
EFM Strip Retention After Legacy Perinatal System Replacement
Often, when a perinatal system gets replaced, only discrete charting data like assessments and vitals is migrated into the hospital’s new EHR (i.e., Epic or Cerner). That leaves fetal monitoring strips to be archived elsewhere for future accessibility. Providing that access, however, can be challenging.
Fetal monitoring strips are frequently displayed by the legacy perinatal system in a graphical interface. That means that when the data is extracted from the system in which it resides and displays, it is often in an unusable format. This leaves providers with only a few compliant fetal monitoring strip retention options:
- Keep the legacy perinatal software in full production (or read-only mode). The main issue with this solution is the maintenance cost to keep a replaced system up and running with the sole purpose of storing fetal monitoring strips. It also poses technical and security risks as the system ages.
- Pay the legacy vendor to provide fetal monitoring strip output to PDF. The challenge with this option often starts with the cost. The legacy vendor is in a situation to charge what hospitals may consider to be an excessive amount to generate the needed output from the fetal monitoring software. And, once it is generated, the protected health information must be indexed and stored in a HIPAA-compliant manner, somehow linking the strips to the rest of the patient’s medical record data.
- Preserve the fetal monitoring strips in a secure archive that offers SSO to the EHR. Harmony Healthcare IT, the top data extraction and migration healthcare IT company according to Black Book™ Rankings and the makers of HealthData Archiver®, offer a proprietary solution that is built to provide a searchable fetal monitoring strip directory organized by patient. And, to connect the strips to the rest of the medical record, Single Sign On (SSO) functionality to leading EHRs like Epic, Cerner, Allscripts and athenahealth is offered. That makes for a secure, cost-effective, HIPAA-compliant and long-term legacy data management strategy for fetal monitoring strips.
At Harmony Healthcare IT, data availability for the full clinical narrative of the patient is a top priority. And that includes the critical fetal monitoring strips from the youngest patients in your care.
Are you seeking data archive solutions and a legacy system replacement strategy for perinatal systems like Phillips OB TraceVue, GE Centricity™ Perinatal, PeriGen Watchchild®, OBIX fetal monitoring or others? Need to make sure all your data retention requirements, including fetal monitoring strips, can be met for the long haul of 28 years or more?
We are the team to help you. Let’s talk.







